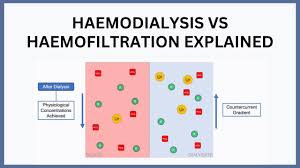
Renal replacement therapy (RRT) is one of the cornerstones of modern medicine for patients with end-stage renal disease (ESRD) or severe kidney failure. As kidney function declines, the body loses the ability to remove toxins, excess fluid, and waste products. This is where extracorporeal blood purification therapies—most commonly hemodialysis (HD) and hemodiafiltration (HDF)—play a life-sustaining role.
Although both therapies share the same fundamental purpose—cleansing the blood—they differ significantly in mechanism, efficiency, clinical outcomes, and treatment experience. Over the past two decades, hemodiafiltration has gained attention due to evidence suggesting improved clearance of middle-molecular-weight toxins and potential survival benefits. Meanwhile, traditional hemodialysis remains widely available, highly standardized, and cost-effective for millions of patients worldwide.
In addition to these mainstream therapies, other extracorporeal purification methods such as hämoperfusion, as well as complementary wellness-oriented interventions like ozone therapy, are sometimes discussed in the context of detoxification or adjunctive treatment. While these modalities do not replace dialysis, they contribute to the broader landscape of blood purification technologies.
This article provides an in-depth, human-style explanation of the differences between hemodialysis and hemodiafiltration, why each is used, the types available, treatment steps, benefits, and frequently asked questions. Whether you are a student, a patient, or a professional seeking structured academic content, you will find this comprehensive guide both accessible and scientifically grounded.
Why Understanding the Difference Matters
Understanding how hemodialysis differs from hemodiafiltration is important for several reasons:
- Better Treatment Decision-Making
Patients and families are often faced with choosing between available therapy options. Knowledge of how each method works allows for more informed discussions with healthcare providers.
- Different Mechanisms = Different Clinical Outcomes
Hemodialysis mainly uses diffusion, whereas hemodiafiltration uses both diffusion and convection. These mechanisms influence how effectively different toxin sizes are removed.
- Potential Survival Benefits
Some clinical studies suggest that high-volume HDF may reduce mortality rates in long-term dialysis patients. Understanding this is valuable for assessing long-term treatment strategies.
- Understanding Costs and Accessibility
Hemodialysis machines are cheaper and widely accessible, while hemodiafiltration requires advanced equipment and high-quality water systems. This affects treatment availability across regions.
- Relation to Other Blood Purification Techniques
Comparing dialysis with selective therapies such as hämoperfusion or wellness approaches like ozone therapy helps place each treatment in the broader context of physiological detoxification and modern medical technology.
What Is Hemodialysis?
Hemodialysis is the most common kidney replacement therapy, used worldwide in hospitals, dialysis centers, and increasingly in home-based settings.
Definition
Hemodialysis is a process where a machine filters a patient’s blood to remove toxins, fluid, and electrolytes through diffusion across a semi-permeable membrane.
How It Works
- Blood flows from the patient to a dialyzer (artificial kidney).
- Inside the dialyzer, blood flows along one side of a membrane.
- Dialysate fluid flows along the other side.
- Waste products diffuse from the blood into the dialysate.
- Clean blood returns to the patient.
Key Mechanism: Diffusion
Diffusion removes small molecules efficiently—like:
- Urea
- Creatinine
- Potassium
- Sodium
However, diffusion alone is less effective for middle-molecular-weight toxins, which are increasingly recognized as harmful in long-term dialysis patients.
What Is Hemodiafiltration?
Hemodiafiltration (HDF) is a more advanced form of dialysis that combines both diffusion (like standard HD) and convection, allowing for more efficient toxin removal.
Definition
Hemodiafiltration is a hybrid dialysis therapy that simultaneously uses diffusion and convection to remove small, middle, and some larger molecules from the bloodstream.
How It Works
- Blood is filtered through a membrane.
- A large volume of plasma water is removed via convection.
- This “ultrafiltration” drags solutes along with it, clearing larger molecules.
- The removed volume is replaced by sterile substitution fluid.
- Diffusion continues simultaneously to clear small solutes.
Key Mechanism: Convection
Convection improves removal of:
- Beta-2 microglobulin
- Middle-molecular-weight uremic toxins
- Some inflammatory mediators
Patients often describe HDF as a more “gentle” therapy, with fewer blood pressure drops and better post-dialysis energy levels.
Key Differences Between Hemodialysis and Hemodiafiltration
|
Feature |
Hemodialysis (HD) |
Hemodiafiltration (HDF) |
|
Primary mechanism |
Diffusion |
Diffusion + Convection |
|
Toxin removal |
Small molecules |
Small + middle molecules |
|
Efficiency |
Standard |
High-performance |
|
Water quality requirements |
Standard |
Ultra-pure water required |
|
Post-treatment recovery |
Moderate |
Often improved |
|
Cost |
Lower |
Higher |
|
Equipment |
Widely available |
Advanced machines required |
|
Clinical benefit |
Effective |
Potentially better long-term outcomes |
Types of Hemodialysis
Hemodialysis comes in various forms depending largely on treatment frequency, location, and machine technology.
- Conventional In-Center Hemodialysis
- 3 times per week
- 3–5 hours per session
- Most common worldwide
- High-Flux Hemodialysis
Uses a high-flux membrane for better middle molecule clearance (a step closer to HDF).
- Home Hemodialysis
Growing rapidly, allowing:
- Short daily sessions
- Nocturnal long sessions
- Slow Low-Efficiency Dialysis (SLED)
Used for critically ill patients in ICU.
Types of Hemodiafiltration
HDF has more technical variations based on how substitution fluid is delivered.
- Pre-Dilution HDF
Substitution fluid enters before the dialyzer.
- Easier on the filter
- Slightly less efficient due to dilution
- Post-Dilution HDF
Substitution fluid is added after passing through the filter.
- Most efficient
- Requires high blood flow rates
- Mixed Dilution HDF
Combines both pre- and post-dilution to maximize toxin removal while preventing filter clogging.
- High-Volume HDF
- Most effective form
- Requires >20–25 L of convection volume per session
- Associated with potential survival benefits
Advantages and Benefits of Hemodialysis
- Widely Available
Most healthcare systems can provide HD, making it accessible to nearly all kidney failure patients.
- Cost-Effective
Less expensive machines and lower water purity requirements.
- Effective Small-Molecule Clearance
Excellent at removing urea, creatinine, and electrolytes.
- Flexible Scheduling
Patients can choose between:
- In-center sessions
- Home sessions
- Short daily or long nightly treatments
- Rapid Correction of Electrolyte Imbalance
Particularly important in:
- Hyperkalemia
- Severe metabolic acidosis
Advantages and Benefits of Hemodiafiltration
- Superior Middle-Molecule Removal
HDF’s convection process removes molecules that HD struggles with, including inflammatory toxins.
- Improved Hemodynamic Stability
Patients often report:
- Fewer blood pressure drops
- Less cramping
- Better tolerance during treatment
- Reduced Inflammation and Oxidative Stress
Some studies link HDF to decreased systemic inflammation.
- Better Clinical Outcomes
Potential benefits include:
- Reduced hospitalization
- Lower cardiovascular stress
- Improved long-term survival (especially with high-volume HDF)
- Enhanced Quality of Life
Many patients report better:
- Energy levels
- Appetite
- Sleep quality
- Overall well-being
Where Hämoperfusion and Ozone Therapy Fit In
While hemodialysis and hemodiafiltration are mainstream medical practices, hämoperfusion and ozone therapy occupy a different space within the landscape of blood purification.
Hämoperfusion
Hämoperfusion involves passing blood through a cartridge filled with adsorbent material (e.g., activated charcoal, resins).
Common uses:
- Poisoning (drug overdose)
- Removing specific toxins not effectively cleared by dialysis
- Sepsis adjunct therapy (in some settings)
It is not a replacement for dialysis but is sometimes combined with HD or HDF for specific indications.
Ozone Therapy
Ozone therapy is not a dialysis method but an alternative wellness therapy sometimes promoted for:
- Immune modulation
- Detoxification
- Anti-microbial properties
It is not a mainstream medical substitute for renal replacement therapy but is occasionally discussed alongside blood-related therapies.
Step-by-Step Procedure: Hemodialysis vs Hemodiafiltration
The patient experience is similar for both therapies, but the underlying technology differs.
Steps in Hemodialysis
- Vascular Access
Either:
- Arteriovenous fistula (preferred)
- Graft
- Central venous catheter
- Connecting to the Machine
Nurses connect the patient via bloodlines.
- Blood Pumping
Blood flows at 200–450 mL/min to the dialyzer.
- Diffusion Process
Toxins move across the membrane into dialysate.
- Ultrafiltration for Fluid Removal
Water is removed to reach the patient’s dry weight.
- Completion
Blood lines are disconnected; the patient rests briefly.
Steps in Hemodiafiltration
Most steps mirror hemodialysis with added features.
- Vascular Access
Need for higher blood flow than standard HD.
- Ultra-Pure Water Production
Required for substitution fluid production.
- Convection and Ultrafiltration
Large volumes of plasma water are filtered.
- Substitution Fluid Infusion
Sterile fluid replaces filtered volume.
- Simultaneous Diffusion
Dialysate still removes small solutes.
- Monitoring Convection Volume
High-volume HDF targets >20 L per session.
- Session Completion
Patients often feel less fatigued afterward.
Conclusion
Hemodialysis and hemodiafiltration are foundational therapies for patients with kidney failure, each with distinct mechanisms, benefits, and clinical implications.
- Hemodialysis remains the most widely used, accessible, and effective for small-molecule toxin removal.
- Hemodiafiltration represents a technological evolution of dialysis, delivering enhanced clearance of middle molecules and potential improvements in patient outcomes, especially when used in high volumes.
Understanding the differences helps patients, caregivers, and students make informed decisions. While complementary therapies like hämoperfusion or ozone therapy may appear in broader discussions, they do not replace the essential role of HD and HDF in renal care.
FAQ
- Is hemodiafiltration better than hemodialysis?
HDF often provides better toxin removal and may offer improved survival, but availability, cost, and water quality requirements are limiting factors.
- Why isn’t HDF used everywhere?
It requires ultra-pure water systems and more advanced machines, which some centers cannot provide.
- Does HDF hurt more than HD?
No—patients often feel better during and after HDF, with fewer cramps and blood pressure issues.
- Can hämoperfusion replace dialysis?
No. Hämoperfusion removes certain toxins but cannot remove fluid or electrolytes like dialysis can.
- Is ozone therapy useful for kidney patients?
Ozone therapy cannot replace dialysis but is sometimes used as an adjunct wellness therapy in certain clinics.
- Which therapy removes more toxins?
HDF generally removes both small and middle molecules more effectively than standard HD.
- Can I switch from HD to HDF?
Many patients can, depending on:
- vascular access quality
- available equipment
- medical suitability
- Is HDF more expensive?
Yes, due to equipment and water purity requirements.