Understanding the difference between an endoscopy vs colonoscopy is important for your digestive health. Both procedures examine parts of your gastrointestinal (GI) tract but serve different purposes. Knowing what to expect helps reduce anxiety and ensures you are well-prepared.
This article will explain the key differences, common uses, preparation, procedure details, recovery, and answer frequently asked questions about endoscopy and colonoscopy.
What is an Endoscopy?
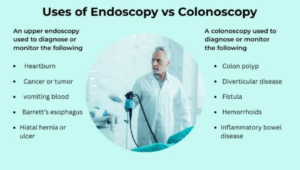
An endoscopy is a procedure that allows your doctor to examine the upper GI tract, including the esophagus, stomach, and the first part of the small intestine. It uses a flexible tube called an endoscope with a camera and light at the tip.
Common uses include:
- Diagnosing acid reflux, ulcers, or gastritis
- Detecting infections or inflammation
- Taking tissue samples (biopsies)
- Removing foreign objects or polyps
The procedure is generally quick, often completed in 15–30 minutes under sedation, and causes minimal discomfort.
What is a Colonoscopy?
A colonoscopy examines the lower GI tract, specifically the colon and rectum. It uses a colonoscope, similar to an endoscope but longer, to inspect for polyps, cancer, and other abnormalities.
Common uses include:
- Screening for colorectal cancer
- Investigating unexplained bleeding or changes in bowel habits
- Diagnosing inflammatory bowel disease (IBD)
- Removing precancerous polyps
Colonoscopy typically takes 30–60 minutes and is done under sedation to reduce discomfort.
Key Differences Between Endoscopy and Colonoscopy
|
Feature |
Endoscopy |
Colonoscopy |
|
Area Examined |
Upper GI tract |
Lower GI tract |
|
Tube Length |
Short |
Long |
|
Common Indications |
Acid reflux, ulcers, gastritis |
Polyps, colorectal cancer, IBD |
|
Sedation |
Moderate to deep |
Moderate to deep |
|
Recovery |
Usually quick |
Few hours due to bowel prep and sedation |
|
Bowel Prep |
Not required |
Required for clear visualization |
The main difference is the section of the digestive tract examined, although both procedures can be used for biopsies and treatment.
Preparation for Each Procedure
Endoscopy Preparation
- Fasting 6–8 hours before the procedure
- Avoid certain medications as advised by your doctor
- Arrange transportation if sedated
Colonoscopy Preparation
- Follow a clear liquid diet 1–2 days before
- Take prescribed laxatives or bowel prep solutions
- Avoid certain foods that may interfere with visualization
- Arrange someone to drive you home after sedation
Proper preparation ensures better visibility and reduces complications.
Procedure Experience
During Endoscopy
- You lie on your side while the endoscope is inserted through your mouth
- Sedation helps you relax and minimizes discomfort
- You may feel mild gagging or pressure
During Colonoscopy
- You lie on your side while the colonoscope is guided through your rectum
- You may feel cramping, pressure, or bloating
- Sedation reduces discomfort significantly
Both procedures are generally well-tolerated, and doctors monitor you closely for safety.
Recovery and Aftercare
Endoscopy:
- Mild sore throat or bloating may occur
- Most patients resume normal activities the same day
- Avoid driving until sedation effects wear off
Colonoscopy:
- Bloating, cramping, or mild gas is common
- Avoid heavy meals immediately after
- Follow up on biopsy or polyp results
Hydration, rest, and following your doctor’s advice help ensure smooth recovery.
Risks and Safety
Both procedures are safe but have potential risks:
- Bleeding: More common with polyp removal
- Perforation: Rare but serious
- Sedation-related reactions: Rare
Your doctor will explain risk factors and safety precautions before the procedure.
Benefits of Endoscopy and Colonoscopy
- Early detection of cancers and precancerous conditions
- Accurate diagnosis of digestive disorders
- Opportunity for treatment during the procedure (biopsy or polyp removal)
- Peace of mind about your GI health
Despite mild discomfort, these procedures are invaluable for long-term digestive health.
FAQ: Endoscopy vs Colonoscopy
- Are endoscopy and colonoscopy painful?
No, sedation minimizes pain; mild pressure or cramping may occur. - Which procedure is better for detecting ulcers?
Endoscopy is preferred for upper GI ulcers. - Which detects colorectal cancer?
Colonoscopy is the gold standard for colorectal cancer screening. - Can I eat before these procedures?
Endoscopy requires fasting; colonoscopy needs bowel prep and clear liquids. - How long do results take?
Biopsy results may take a few days; polyps may require pathology review. - Are these procedures safe?
Yes, with minimal risks when performed by trained professionals. - Can both be done in one visit?
Rarely, as preparation differs for each. - Is sedation necessary?
Not always, but it is recommended for comfort. - How often should I have these procedures?
Depends on age, risk factors, and findings; consult your doctor. - Can polyps be removed during colonoscopy?
Yes, it is one of the main advantages of colonoscopy.